What is circumcision?
Circumcision is the removal of the distal foreskin of the penis. Medical indications include lowered risks of urinary tract or foreskin infection, sexually transmitted disease and penile cancer. It is the treatment for a foreskin that is stuck behind the head of the penis (paraphimosis). The absolute numbers of these risks are low, for example, the risk of urinary tract infection is 1 out of 1,000 patients for circumcised boys, and 1 out of 100 for uncircumcised boys. There are risks of the procedure which are discussed below.
Should my baby boy have a circumcision?
When boys are born, their foreskin is usually unable to be pulled back over the opening of the urinary tract (urethral meatus). This condition, called physiological phimosis or non-retractile foreskin, typically resolves itself with age, with the majority of boys able to retract their foreskin by the time they are five years old.
The decision for circumcision during infancy is a personal one. The American Academy of Paediatrics Circumcision Policy Statement recognizes the health benefits of circumcision but does not deem the procedure to be a medical necessity for the well-being of the child (1). Many parents from America, Australia and Philippines were circumcised when they were newborn and it is culturally acceptable. The Jewish and Muslim religions also propose it to be performed within 7 days of life.
When is the best time for circumcision?
The best time for circumcision remains controversial, and is strongly influenced by religious and cultural beliefs. It is performed during infancy, as a boy or as an adult. In the newborn or infant, the circumcision can be performed without general anaesthesia (GA), hence avoiding general anaesthetic risks. Secondly, there is minimal memory of the procedure having been performed.
In childhood, there is the need for sedation when the child is unable to cooperate and stay still. Conversely, when the child is able to cooperate, the operation can be performed under local anaesthesia, without need for sedation or GA.
Now, my son has grown up and has an infection of the foreskin. Should he have a circumcision?
Your son should be examined by a general practitioner, paediatrician or a paediatric surgeon. During an acute infection of the foreskin, treatment is antibiotics and painkillers. After the infection has settled, I will re-examine your child and advice whether circumcision or topical steroid cream should be used to prevent recurrent infection. The benefits and risks of circumcision are discussed. The circumcision procedure is the definitive treatment to prevent a recurrence.
Topical steroid cream is effective in some patients, which is dependent on patient and caregiver compliance and technique. In uncooperative patients, it is difficult to apply the steroid cream and gently retract the foreskin, hence decreasing the effectiveness of treatment. Varying success is reported from 50 to 90% in the literature (2). It is important to know where and how to use the cream to ensure the highest efficacy. I advise applying for a maximum of 6 weeks, because of the potential side effects of skin thinning, ulceration and infection. Recurrent tightening of the foreskin around the urinary tract opening is concerning for worsening of the condition and scarring (balanitis xerotica obliterans).
How is circumcision performed?
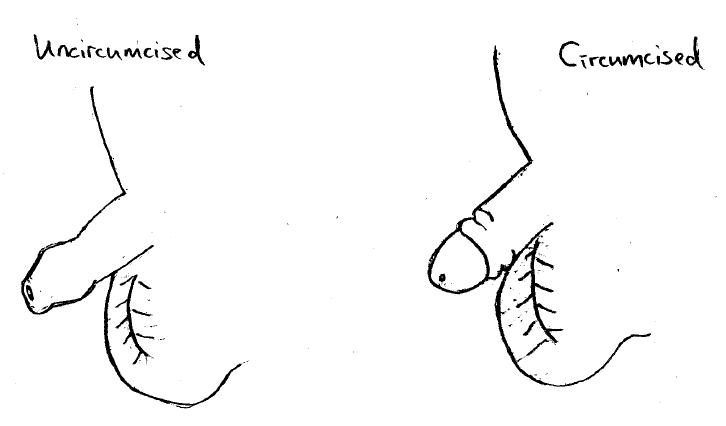
In newborns and babies till 6 months old, circumcision can be performed under local anaesthesia with an energy device. I perform the modified sleeve circumcision instead of the Plastibell ring, because there is less pain, less risk of device dislodgment and subsequent bleeding, and less risk of excess skin causing prepuce adhesions. The baby is awake and has a pacifier for comfort. The foreskin is cleaned under antiseptic conditions. Local anaesthesia is given. A sleeve of foreskin is cut circumferentially around the inner and outer prepuce. Circumcision is completed by trimming the excess skin off, and the edges are sutured together after haemostasis (Figure 1).
In an older boy, I perform a modified sleeve circumcision under local anaesthesia with sedation, or general anaesthesia. The excess foreskin is trimmed and haemostasis is achieved using diathermy or laser, which are energy devices that seals the blood vessels. The outcome of diathermy and laser is the same. The skin is closed with absorbable sutures.
I perform a history and physical examination to identify indications for circumcision and alternative therapeutic options. When needed, there is an anaesthetist, who will provide sedation or general anaesthesia. During the surgery, structural abnormalities may be found during the removal of the foreskin, for example a penile torsion or megameatus intact prepuce. These abnormalities may be corrected in a later surgery under sedation or general anaesthesia. The correction of these abnormalities is not possible when the circumcision is performed under local anaesthesia.
How is the recovery post circumcision:
Please bring along boxer shorts or loose underwear for your child to wear after circumcision. The patient can have normal baths. Washing with tap water or sterile solution after each pee helps keep the wound clean. Minimal bleeding or swelling is expected. Granulation tissue appears as small yellowish areas on or around the head of the penis, because the raw skin is exposed and forms a more mature layer.
In babies, it is advisable to check the diaper 1 to 2 hourly. If the diaper are soiled with pee or poop, please change it to keep the wound clean. A thin layer of Vaseline can be applied to the wound.
If a Plastibell was used, after 3 to 14 days, the Plastibell drops off as the excess foreskin shrivels up. The Plastibell may dislodge too early, resulting in bleeding and unsatisfactory wound healing.
In an older boy, the discomfort improves after the 1st day. The painkillers may be required during the first 2 days after surgery.
The risks of circumcision include bleeding, bruising and infection. Infection presents as increasing pain, redness, swelling, or abnormal discharge from the circumcised site. If any of these occur, treatment is available and we can be contacted at +65 87727527 or +65 63592679. Prepuce adhesions may occur if the child is becomes more chubby because the suprapubic fat pushes the skin forward over the glans penis.
What are the costs for circumcision?
We take reference from the Ministry of Health, Singapore, Fee Guidelines. These fees are payable by Insurance, Medisave, Child Development Account (CDA) and Baby Bonus Cash Gift, when applicable. The costs are fully payable via CDA, claimable from Medisave up to SGD $1250 for a Day Surgery procedure (3), and claimable from insurance when applicable. The procedure is done in our operating theatre at Paediatric Surgery and Urology International Ambulatory Surgical Centre. The total cost for an uncomplicated circumcision includes consultation, medications, use of the ambulatory surgical centre facility, and standard consumables. They are as follows:
The estimated total cost for circumcision in a newborn baby until 3 months old, is SGD $1250 subject to Goods and Services Tax (GST). This is performed under local anaesthesia.
The estimated total cost for circumcision in a child between 3 months to 6 months old, is SGD $2250 subject to Goods and Services Tax (GST). This is performed under local anaesthesia.
The estimated total cost for circumcision in a child between 6 months to 9 months old, is SGD $3250 subject to Goods and Services Tax (GST). This is performed under local anaesthesia.
The estimated total cost for circumcision in a child between 9 months to 12 months old, is SGD $4250 subject to Goods and Services Tax (GST). This is performed under local anaesthesia.
The estimated total cost for a child more than 1 year old, will be SGD $6000 subject to GST. This is performed under sedation or general anaesthesia and local anaesthesia.
When there are complications for example, allergy (not previously known) to medications used, the costs differ.
References
(1) Circumcision policy statement. American Academy of Pediatrics. Task Force on Circumcision. Pediatrics. 1999 Mar;103(3):686–93.
(2) Moreno G, Corbalán J, Peñaloza B, et al. Topical corticosteroids for treating phimosis in boys. Cochrane Database Syst Rev. 2014 Sep 2;(9):CD008973.
(3) https://www.moh.gov.sg/cost-financing/healthcare-schemes-subsidies/medisave
Share if you like this post
If you have other enquiries on children’s surgical conditions, feel free to contact us
© Copyright- 2023 Childsurgery.sg
All Rights Reserved
